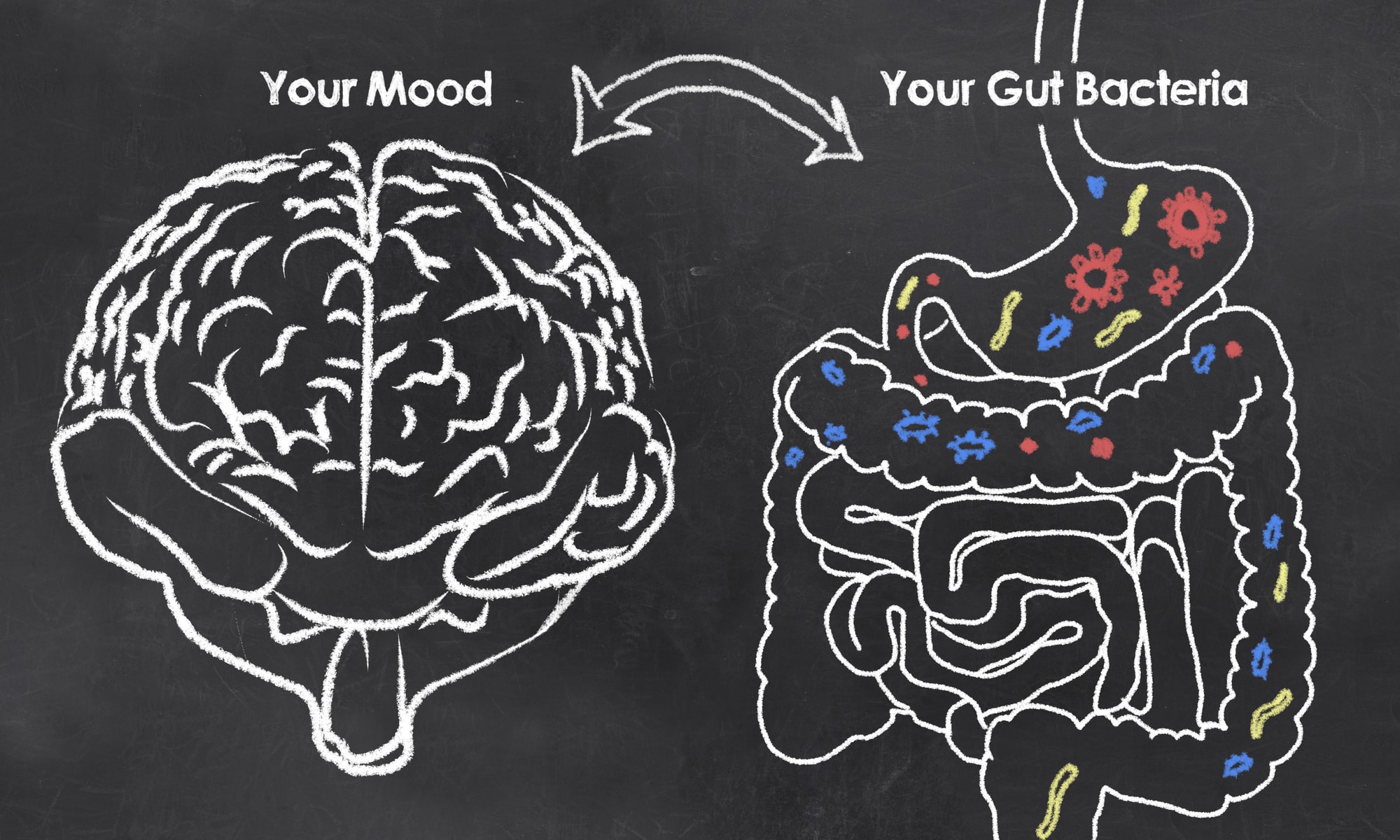
“Trust your gut,” “go with your gut,” “a gut reaction,” – all are idioms which reference to listening to our digestive tract. But do we? And if we are listening, what’s it saying?
Researchers have now begun to call our stomach our “second brain.” Within this brain are millions of neurons communicating with each other and other areas of our body. Our intestinal tract contains millions of bacteria cells or gut microbiota. These microbes, as well as others living in different areas of the body, are known as the microbiome. In fact, our body contains more bacterial DNA than it does human DNA.
Think about that. We are more bacteria than we are human.
But why is our gut our second brain? And what impact does its bacteria have on our mood and wellbeing?
It turns out our gut makes neurochemicals. There is more serotonin, the neurotransmitter most often associated with depression, in our gut than in our brain. In 2014, researchers were able to discern a difference in gut bacteria between those diagnosed with depression and those without. It makes sense when you consider that many mental health disorders, as well as their pharmaceutical treatments, often have gastrointestinal side effects. Research has also shown that the bacteria lactobacilli helps release GABA, the neurotransmitter that helps calm nervous energy and is often related to anxiety disorders.
Unfortunately, while we understand that our gut health and mental health are related, we don’t fully understand how. We do know that bacteria responds to emotional and physical stress. Cortisol, the “stress hormone,” plays a role in this relationship and might be how gut bacteria communicates with the brain.
Research has been able to show that introducing different bacteria changes our behavior, and we aren’t even consciously aware of it. One study has shown that being exposed to certain bacteria early in life can influence whether or not one develops depression or anxiety. Even though the processes and connections between the brain and the gut aren’t fully understood, we do know that having a healthy gut can mean having a healthy mind.
So what can you do to take good care of your gut?
One can infer that taking good care of your intestinal flora will lead to overall wellness. Some research suggests that probiotics will achieve this goal. Unfortunately, we don’t know a great deal about these probiotics. We know that they probably have an impact on our gut flora, but we don’t really know what this means for our gut or for the rest of our body. And we don’t fully know the actual benefits or risks of long-term use. Unfortunately, much of the research on probiotics has been done by the developers of probiotics themselves, and they have a pretty big stake in finding certain results. This is not to say that we should all toss our pills down the drain. But, be aware that a probiotic isn’t the cure-all that it’s marketed to do.
What’s most consistent and promising is a healthy lifestyle. The old adage stands true: you are what you eat. Eating for wellness might not be something we all think about. Oftentimes we end up eating for boredom, comfort, a mood, or a craving. Instead, you can change your relationship with food and think about what will be most nourishing to your wellbeing. Does that pizza look warm and yummy? Sure. But will you feel sluggish and cranky afterward? Yep!
Foods that cause inflammation in your intestines will send a signal to your brain that something isn’t right. This signal can lead to effects such as fatigue, irritability, sadness, and anxiety. Long-term poor eating can lead to long-term inflammation, which can then lead to long-term mood disturbances such as anxiety and depression. Thinking about eating for mental health and wellness might positively change your choices.
To start, try eliminating foods that are known to cause inflammation: sugar, dairy, wheat, processed foods, refined flours, artificial sweeteners, artificial additives, alcohol, and processed meats. Implementing an elimination diet might be a good option to discern what food sensitivities you might have. You can also keep a food journal to track your mood after your meals. Sometimes our mood can change long after we eat a meal due to the digestion process, so be mindful of this. Additionally, eating foods that are fermented such as sauerkraut, kefir, and tempeh have shown to improve our gut flora.
Changing your diet will change the microbes in your gut and will thus change your behavior and mood.
Research also shows that stress plays a huge role in our immune system and healthy gut bacteria. Bacteria responds to emotional and physical stress. Making sure that self-care is a top priority and coping with daily life stressors is a great way to ensure a healthy gut.
Studies are currently looking at how introducing different bacteria can alter or change our behavior. Fecal transplants (as cringe-worthy as they sound) show promise into helping conditions such as Alzheimer’s disease, multiple sclerosis, and autism. This might be where the future of mental health is going. However, until we are there, eating well, exercising, getting good sleep, and managing our stressors are still the best pathways to health and wellbeing.